What does it look like
Pink skin
Main body location
All over / Widespread, Arm, Back, Chest, Face, Hand, Head, Leg, Trunk
Can it appear anywhere?
Yes
Find your nearest clinic
Explore our interactive mapMelanoma
What is Melanoma?
What does it look like
Pink skin
Main body location
All over / Widespread, Arm, Back, Chest, Face, Hand, Head, Leg, Trunk
Can it appear anywhere?
Yes
Find your nearest clinic
Explore our interactive mapWhat causes melanoma?
The most important preventable cause is exposure to too much ultraviolet light in sunlight, especially during the first 20 years of life. There is lots of evidence linking melanoma to this, and melanomas are especially common in white-skinned people who live in sunny countries. The use of artificial sources of ultraviolet light, such as sun beds, also raises the risk of getting a melanoma.
Some people are more likely to get a melanoma than others:
- People who burn easily in the sun are particularly at risk. Melanoma occurs most often in fair-skinned people who tan poorly. Often they have blond or red hair, blue or green eyes, and freckle easily. Melanomas are less common in dark-skinned people.
- Past episodes of severe sunburn, often with blisters, and particularly in childhood, increase the risk of developing a melanoma. However, not all melanomas are due to sun exposure, and some appear in areas that are normally kept covered.
- People with many (more than 50) ordinary moles, or with a very large dark hairy birthmark, have a higher than average chance of getting a melanoma.
- Some people have many unusual (atypical) moles (known as 'dysplastic naevi'). They tend to be larger than ordinary moles, to be present in large numbers, and to have irregular edges or colour patterns. The tendency to have these 'dysplastic naevi' can run in families and carries an increased risk of getting a melanoma.
- The risk is raised if another family member has had a melanoma.
- People who have already had one melanoma are at an increased risk of getting another one.
- People with a damaged immune system (e.g. as a result of an HIV infection or taking immunosuppressive drugs, perhaps after an organ transplant) have an increased chance of getting a melanoma.
Is melanoma hereditary?
About 1 in 10 of people with a melanoma have family members who have also had one. There are several reasons for this. Fair skin is inherited; dysplastic naevi can run in families, as can a tendency to have large numbers of ordinary moles. There have been some gene abnormalities that are associated with an increase risk of melanoma. They are rare and do not make a significant contribution to the overall number of cases diagnosed a year.
What are the symptoms of melanoma?
Melanomas may not cause any symptoms at all, but tingling or itching may occur at an early stage. Some melanomas start as minor changes in the size, shape or colour of an existing mole (see below): others begin as a dark area that can look like a new mole. Later on a melanoma may feel hard and lumpy, and bleed, ooze or crust up.
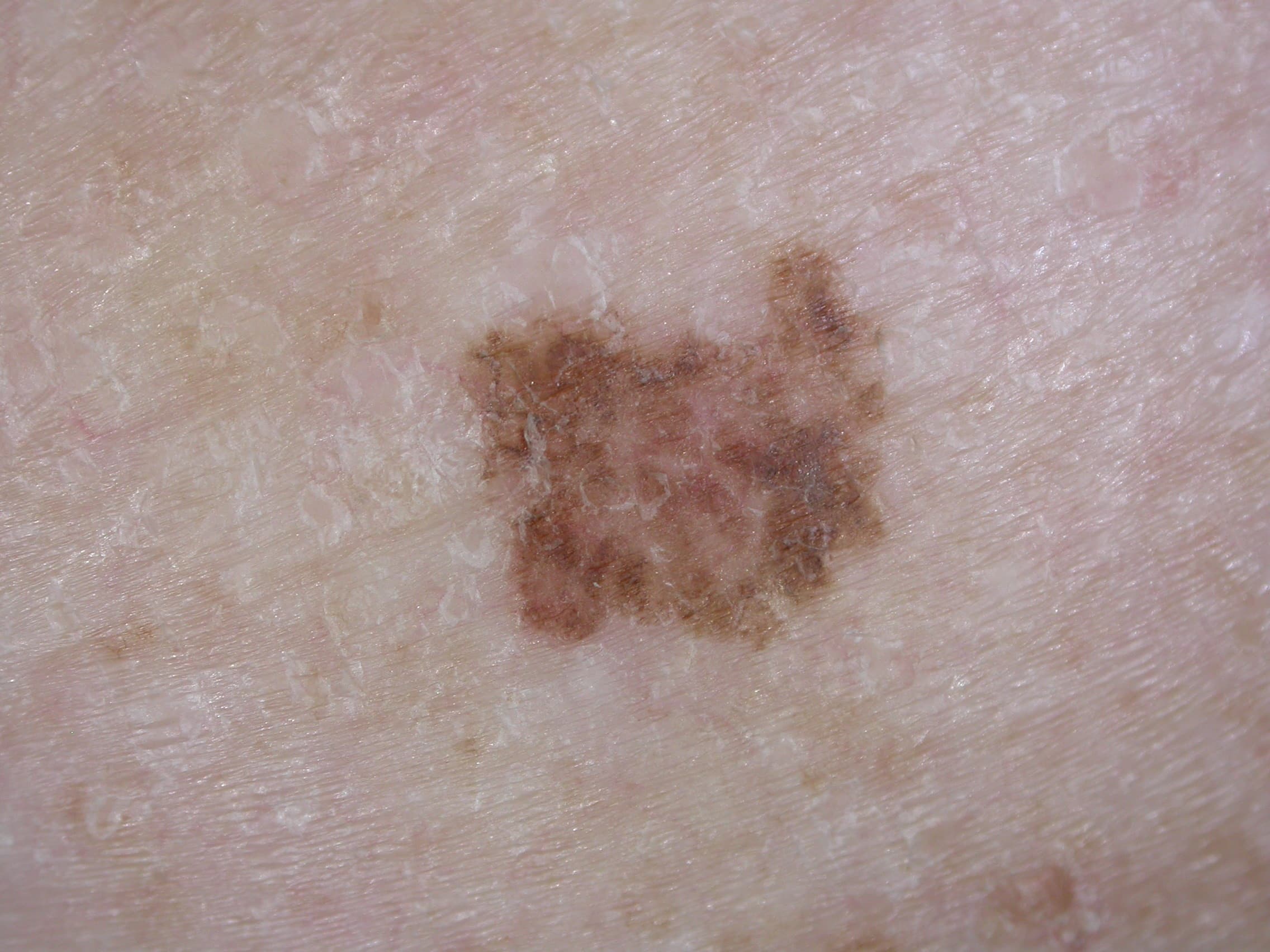
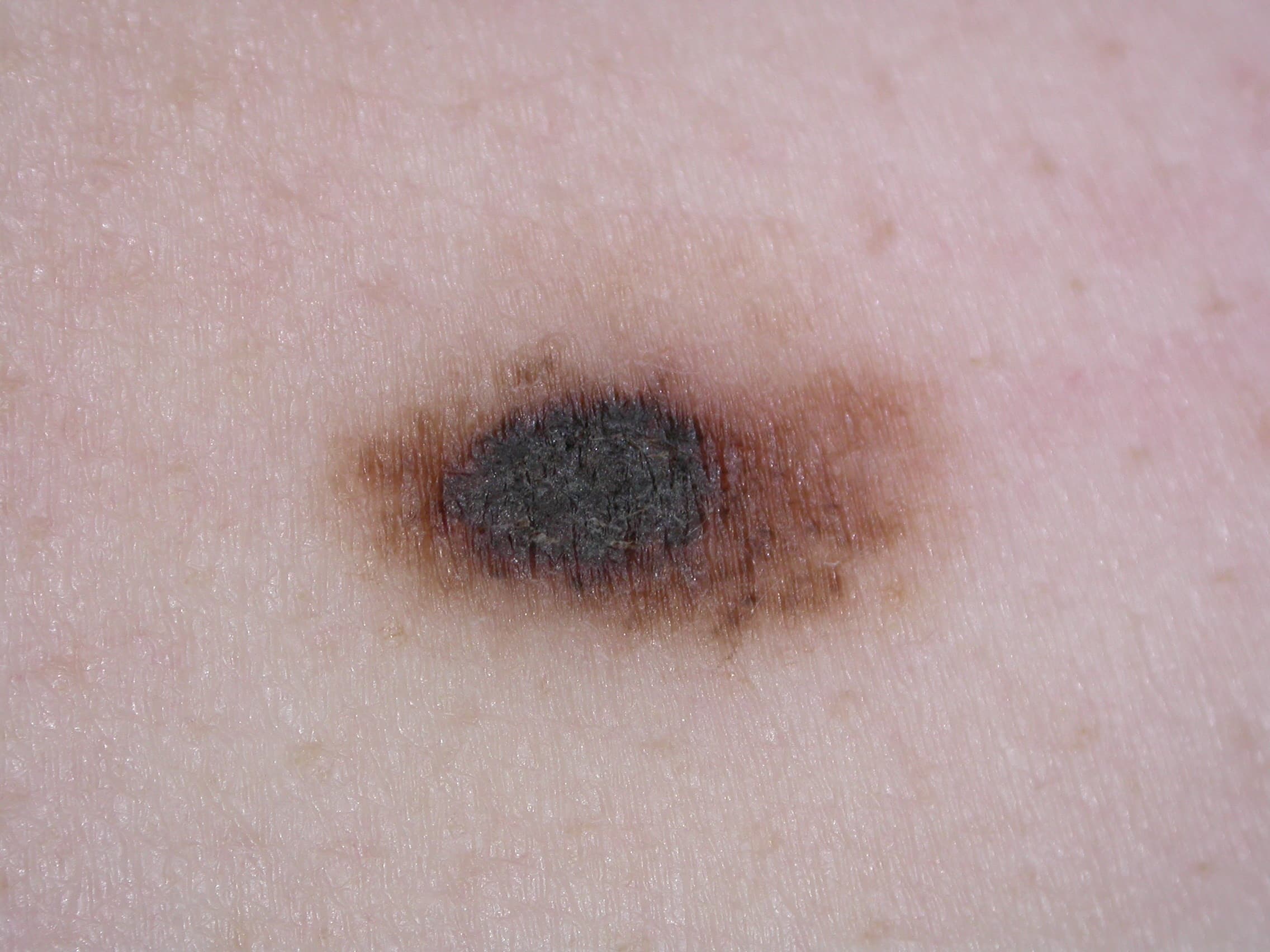
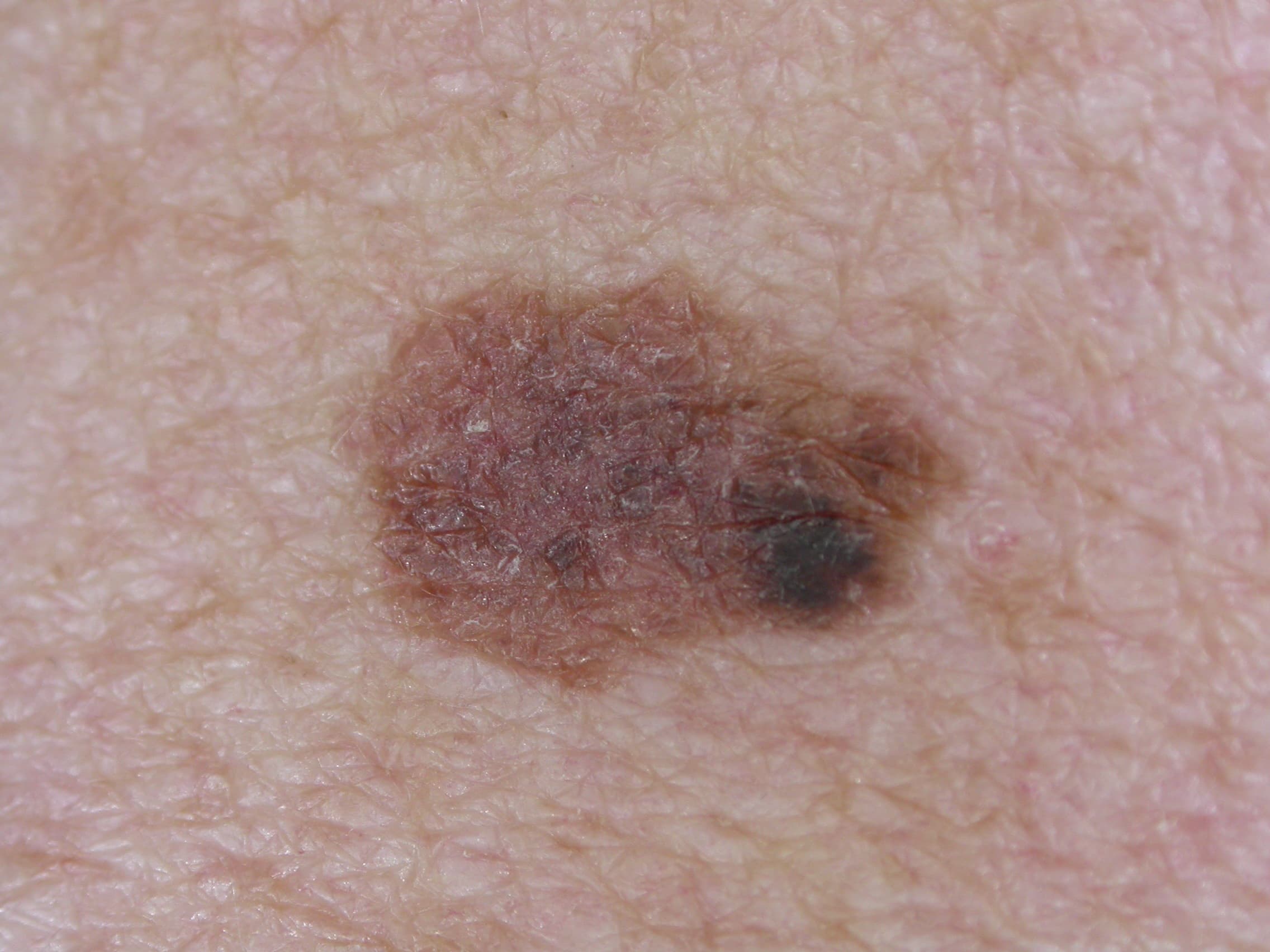
What does a melanoma look like?
All melanomas do not look the same, and there are several different types. The ABCD system (below) tells you some of the things to look out for.
A melanoma may show one or more of the following features:
- Asymmetry – the two halves of the area differ in their shape.
- Border – the edges of the area may be irregular or blurred, and sometimes show notches.
- Colour – this may be uneven. Different shades of black, brown and pink may be seen.
- Diameter – most melanomas are at least 6 mm. in diameter.
Melanomas can appear on any part of the skin but they are most common in men on the body, and in women on the legs.
Images DermNetNZ and Dr Jonathan Bowling.
How is a melanoma diagnosed?
The clinical diagnosis of melanoma is usually made by a specialist (normally a dermatologist or plastic surgeon) by looking at the skin. The initial treatment for a suspected melanoma is to cut out (excise) all of the melanoma cells. Usually this is a minor operation done under a local anaesthetic (via an injection to numb the skin). When the lesion is first removed, although your specialist may feel that it is likely to be a melanoma, the diagnosis needs to be confirmed by examining the tissue removed under a microscope, so the excision is usually done with narrow margins (a thin rim of normal skin around the suspected melanoma). The specimen that is cut out from the skin is sent to a laboratory, so that a pathologist can examine it under the microscope and then confirm if it is a melanoma or not.
Can a melanoma be cured?
Yes: the majority of the people who have a melanoma removed will have no further problems. However it is crucial for a melanoma to be removed as early as possible – before it has had time to spread deep into the skin or to other parts of the body. The thinner the melanoma is when it is removed; the better is the survival rate. This is why a doctor should examine anyone with a suspicious mole or blemish as soon as possible. In a small minority of people the melanoma may have spread but further surgery or chemotherapy can often help to control this.
How is Melanoma Treated
For more information on each stage of melanoma, including treatments please follow these links.
Melanoma Stage 1A
Melanoma Stage 1B
Melanoma Stage 2
Melanoma Stage 3
Melanoma Stage 4
Find your nearest clinic
Use our interactive map to find private dermatologists and clinics in the UK & ROI nearest to where you live.
Related content
Hair loss / Hair problems
Alopecia areata
4 minutes read time
Lump / Lumps / Lumpiness
Basal cell carcinoma
4 minutes read time
Lump / Lumps / Lumpiness
Bowen's disease
3 minutes read time
Blisters / Blistering
Congenital erythropoietic porphyria
4 minutes read time
Blisters / Blistering
Contact dermatitis
5 minutes read time
Hard skin
Darier's disease
4 minutes read time